Telehealth & Pain

Telehealth, the use of digital information and communication technologies to access healthcare services remotely, has become increasingly important for managing and treating patients in pain. Pain is considered to be chronic if it lasts or comes and goes (recurs) for more than three months. Here are five ways telehealth can be utilized to help these patients:
- Remote Consultations with Specialists: Patients suffering from chronic pain or specific pain conditions can use telehealth to consult with specialists who may not be available in their immediate geographic area. This is particularly beneficial for those living in rural or underserved regions, where access to pain management clinics or specialists is limited. Through video conferencing, patients can receive diagnoses, discuss treatment options, and have follow-up appointments without the need for travel, reducing physical discomfort and stress.
- Virtual Physical Therapy and Rehabilitation: Telehealth platforms enable physical therapists to guide patients through exercises and rehabilitation programs remotely. This is crucial for patients who are in pain and may find it difficult to leave their homes for physical therapy sessions. Therapists can demonstrate techniques, monitor patients’ progress in real-time, and adjust exercises or routines as needed, all through video calls. This approach ensures that patients receive consistent and personalized care, which can be pivotal in their recovery process.
- Access to Psychological Support: Chronic pain is not just a physical condition; it has significant psychological effects, including anxiety, depression, and stress, which can exacerbate pain. Telehealth provides a conduit for patients to access psychological support and therapies, such as cognitive-behavioral therapy (CBT), from the comfort of their homes. This ease of access can encourage more patients to seek the help they need, improving both their mental health and their ability to manage pain.
- Medication Management and Prescription Renewals: Managing medications is a critical component of pain management for many patients. Through telehealth, healthcare providers can review a patient’s medication regimen, adjust dosages, and renew prescriptions as necessary. This remote monitoring and management can help prevent medication overuse, address side effects promptly, and ensure that patients have access to their necessary pain relief medications without requiring in-person visits.
- Education and Self-Management Resources: Telehealth platforms offer a wealth of resources for patient education, teaching individuals about their conditions, pain management strategies, and lifestyle modifications that can mitigate pain. These resources can be personalized to the patient’s condition and needs, and they empower patients to take an active role in managing their pain. Interactive tools, webinars, and educational materials can help patients understand their pain, learn new coping strategies, and adhere to their treatment plans more effectively.
In summary, telehealth can significantly improve the quality of life for patients with chronic pain by offering personalized, accessible, and comprehensive care options. By addressing the physical, psychological, and educational needs of patients remotely, telehealth can play a crucial role in the holistic management of this complex condition.
























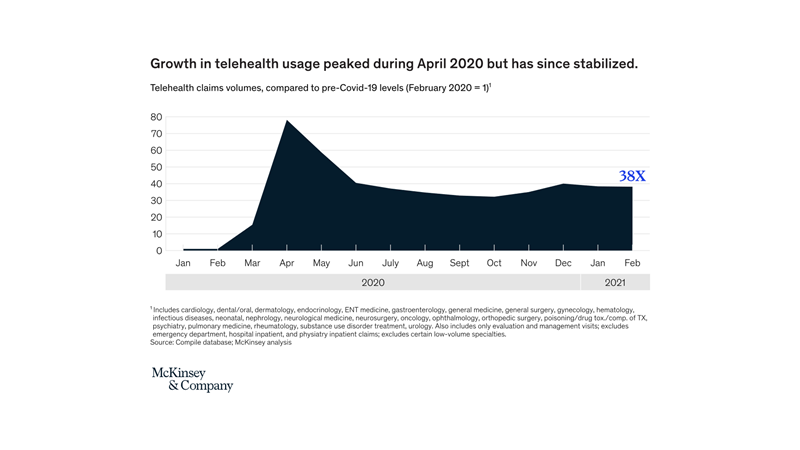




 Thanks Seema Verma, then the CMS administrator, who in April 2020 declared, “the genie out of the bottle on this one”. 1
Thanks Seema Verma, then the CMS administrator, who in April 2020 declared, “the genie out of the bottle on this one”. 1
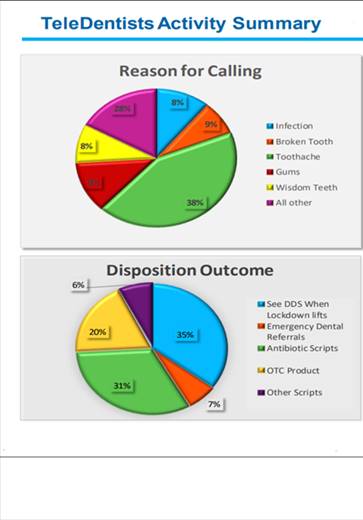
 I’m feeling pretty good. It’s two weeks past my second Covid-19 vaccine. It’s gotten me thinking. When will I no longer need to wear my mask in a crowd? And what will this mean for teledentistry?
I’m feeling pretty good. It’s two weeks past my second Covid-19 vaccine. It’s gotten me thinking. When will I no longer need to wear my mask in a crowd? And what will this mean for teledentistry?

 We live in unprecedented stressful times. There is a global pandemic with no announced cure. Unemployment in the U.S. is at historic levels. Working parents need to supervise remote learners while trying to do their own jobs remotely. Racial tensions have gripped the country. Adult children with parents in nursing homes may not be able to visit. A national election is days away with a tremendous amount of anxiety on all sides. The list goes on.
We live in unprecedented stressful times. There is a global pandemic with no announced cure. Unemployment in the U.S. is at historic levels. Working parents need to supervise remote learners while trying to do their own jobs remotely. Racial tensions have gripped the country. Adult children with parents in nursing homes may not be able to visit. A national election is days away with a tremendous amount of anxiety on all sides. The list goes on.
 Telemedicine has been with us for sixty years.1 The Covid-19 pandemic of 2020 has brought this capability to the forefront as it is now an accepted component for the delivery of healthcare expertise.
Telemedicine has been with us for sixty years.1 The Covid-19 pandemic of 2020 has brought this capability to the forefront as it is now an accepted component for the delivery of healthcare expertise.
 What has changed for teledentistry since the onset of Covid 19? In a word, everything.
What has changed for teledentistry since the onset of Covid 19? In a word, everything.